 Denise Wiesner, LAc, FABORM, is the author of Conceiving with Love: A Whole-Body Approach to Creating Intimacy, Reigniting Passion, and Increasing Fertility. The founder of the Natural Healing and Acupuncture Clinic in West Los Angeles, Wiesner is an internationally recognized traditional Chinese medicine practitioner, specializing in the Whole Systems Chinese medicine approach to women’s health, sexuality, and fertility. Below, read her touching take on dealing with the feelings that arise when we fail to conceive. 10 Ways to Deal with Disappointment When Trying to Conceive Disappointment affects us all. There are no exceptions. Perhaps you are struggling with trying to have a baby, and the immense disappointment that can come from yet another negative pregnancy test or a failed fertility treatment. Whatever the cause of your disappointment, this post may help you. I was cleaning with my bookkeeper and finally got around to organizing my big grey file cabinet – the home of many loose papers in untitled folders that I had been avoiding for years. Endless receipts and warranties for Walkmans (a relic from the 80’s), video cameras, and old TVs were tossed into my throwaway pile. But then I came across a green folder of my writings, and as I flipped through the folder, one piece caught my attention. It was called “Pregnancy Preparation and Disappointment.” I began to read this piece out loud to my bookkeeper, who just three months prior to our meeting, lost her 53-year-old husband to complications of Multiple Sclerosis. Even though the piece was about pregnancy preparation, its words of wisdom were applicable to loss in general, and as I read, tears streamed down her face. It was a poignant moment, as the ending had been written by my late husband, Alex, whose words touched both of us deeply. From 2006: One of my patients who had done her second IVF had just gotten news that it didn’t work. Her Doctor told her it was implantation issues. I wondered if anyone really knew why a pregnancy happened or didn’t happen. I realized that I needed to remind myself about life’s lessons, including disappointment, so I could help my patient. Just then, my four-year-old walked into the room and exclaimed: “I am going to win my soccer game.” I asked him: “What happens if you don’t win?” To which he replied with a flat definition of losing. So I rephrased my question, “How do you FEEL when you don’t win?” He shrugged his shoulders and said, “Nothing.” Out of the mouths of babes. It clearly wasn’t going to ruin his day if he lost. Four-year-olds have a way of just moving on. As Martin Luther King, Jr. said so eloquently, “We must accept finite disappointment, but never lose infinite hope.” That’s a big truth to live by. Here are my ten tips for dealing with disappointment when trying to conceive:
0 Comments
TJ Peyten is a Georgia native with a mission to raise awareness about Male Factor Infertility. She has a background in English, communications, health education, public health, and social work.
TJ's infertility journey started in 2013, when, after five years of marriage, it was discovered that her husband was the factor in their inability to conceive. Frustrated at the lack of support and resources available for those struggling with Male infertility, TJ used her journal as an outlet to deal with the pain. After several years of coping with their infertility through her journal, she finally got the courage to share her story with the world through her book: Semen Secrets: Truths and Confessions A Wife's Journey Through Male Infertility. Visit www.semensecrets.com to learn more. Semen Secret: You can only grieve over the death of a person, or maybe even a pet. When people die, their loved ones grieve. But, in my case, no one died. A few hours after I hung up with the nurse at the lab, the phone rang again. It was my husband. I had been screaming and crying so much that there was no disguising the anguish in my voice. “What’s wrong? Did the doctor say something bad?” I hesitated, “Well, I think we should wait until you get home to talk about this.” “What do you mean?” I could hear the panic in his voice, “Just tell me now. It can’t be that bad. What is it? I only have a few thousand sperm instead of a million?” “I just think we should talk about this at home.” “I got to get back to work. Just tell me!” He was trying not to raise his voice, but his frustration was apparent. I tried to fight back the tears, but they streamed down my face. Choking, I said, “You don’t … you don’t have any have sperm.” “Huh?” I cleared my throat, “I said they didn’t find any sperm, not one. Your semen didn't have any.” There was a long pause, as if time stood still. “Are you going to be okay?” I asked, “I’m so sorry. We can just pray and—" “Please,” he interrupted. “It’s okay. I’m good. I’ll see you when I get home.” For the next several hours I sat alone in silence. My mom called to chat. It was our usual routine, only this time while I was talking, I was still shrouded in silence because I couldn’t hear the words I was speaking. She said I sounded strange. I told her I had a lot going on with work. I didn’t know how to tell my mom that she may not have grandchildren from her only daughter. I waited for the nurse to call me back to tell me it was a mistake. She never did. I went over her words again and again. No sperm. Each time it made tears swell, and I felt a terrible loss of the visions and dreams I had for my family, the plan, our baby. I tried to imagine what I would say to my husband when he got home. Would I grab him and tell him I love him and I’m sorry? Would we cry together? Would I accuse him of ruining our perfect lives? Would I say nothing at all? I wasn’t sure what he would need from me, but in all honesty, I had nothing to give. When my husband came home that evening, he walked in the door like our world was still right-side-up. He put down his bag, looked at the mail, used the bathroom, washed his hands, and went in the fridge to get a snack. I was confused and angry. Here I was agonizing about how I was going to comfort him. We were just told we would never be able to have a child of our own and he felt… nothing? I realized that while I was trying to figure out how to comfort him, I needed him to comfort me. I wanted him to run in and take me in his arms and cry with me until we were spent and exhausted. I would have accepted him yelling in a furious rage, ranting about the unfairness of the situation. But I couldn’t understand him not having a reaction. Finally, we sat down at the kitchen table to talk through the unspeakable. I had to repeat it more than once in my mind before the words would come out of my mouth: “She said they didn’t find any sperm. The doctor wants to set up an appointment with you to go over everything.” His response was immediate, “Well, I don’t want to go. I don’t want to. I don’t have any sperm. That’s it. You want a baby. I can’t do that, so that’s it.” That’s it? That’s it? What do you mean? I began to rock back and forth, shaking my head in disbelief. I looked away trying to hide my hurt and anger as tears began to swell in the corner of my eyes. I wanted to grab him and tell him that I wasn’t going to give up so easily. I wanted to bang on the table, stand up in the chair, and scream until my throat burned. We don’t quit! That’s not it for me! That’s not it for us. Damn it, you gotta have something in there. I just won’t believe it. Instead, I said, “But I didn’t marry you just for a baby.” Although I did expect that was part of the package, “I married you because I love you. You’re my best friend, not just my husband. So, don’t say that.” Before I could finish, the tears that had been building since he walked through the door were flowing down my cheeks. If he wasn’t going to cry, I was. They were not silent, sad tears. These tears were heavy with loss and confusion and regret and anger and hurt and a myriad of other feelings I hadn’t yet identified. My chest heaved, and my head ached. My shoulders shook with the sobs and my face was distorted with all the emotion I couldn’t voice. My husband’s face softened, he reached his hand across the table to comfort me. “Okay,” he said in a whisper. “I’ll go to the follow-up appointment with the doctor,” and then he added, more firmly, “but then we are done with it.” For the remainder of the night, we moved in an awkward silence that was so loud I couldn’t stand it. I drew myself a warm bath and played soft music hoping to reason my way out of this situation, or at least find solace. I stayed in the water until my skin was milky and shriveled, still I had no answers. I wanted to talk to someone who could help me make sense of this or at least offer me the sympathy my husband couldn’t. But also, I couldn’t imagine telling anyone. It felt so shameful. We are supposed to have children. Why us? Why him? Why me? The next morning came and I wasn’t ready to face the day, let alone work. I was worlds away. I kept replaying the phone call in my head. No sperm. That night my husband and I moved in silence again. We avoided each other. When he came to the kitchen, I went to the couch. Instead of watching our favorite shows together, we watched them in separate rooms. When it was time for dinner we tried to make small talk. “How was work today?” “Did you get a chance to go to the store this afternoon?” Eventually, the conversation felt so forced that we stared at our plates and stuffed our faces so could get up from the table and resume ignoring each other. All I could envision was the way we use to laugh and cuddle with one another, follow each other from room to room so we could talk about the day—that was just two days ago. I knew love didn’t fade away that fast, but at that moment my husband felt like a stranger. After dinner, I went outside and cried. It was a cool night and I sat alone under the stars with a glass of wine and some music to keep me company. The salt of the tears mixed with my wine. I kept imaging the life I wanted: us going to the ultrasound, him feeling the baby kick in my stomach, how our parents would react when we told them we were having a baby. I pictured the hospital room—him holding my hand telling me to push. I looked in the backyard and could see the swing set and us running around the yard playing with our child. I tried to convince myself that I was being silly crying over semen, over sperm, or the lack thereof. Those little things that were to carry our DNA did not exist for us. Our children did not exist. I grieved over his semen, my empty womb, our marriage, and our non-existent children, but also the death of my husband’s bright spirit. The light in his eyes grew dim. He became a stranger to himself, to me. I knew he struggled with his thoughts of manhood, but he refused to speak about it. I wanted to help him, to fix it, to fix us. I watched his spirit slip away without understanding how to help him. I wanted to talk about it (as most women do), but he dismissed me every time. And as helpless as I felt, I was also angry that he didn’t try to fix me. I needed him to help me understand all of this. He always helped me figure out what was next. Where was that guy when I needed him? The third night after the call, my husband rolled over in the bed and tapped me gently on my shoulder. I turned towards him, relieved that he was ready to talk. I had longed for his touch and I was eager to embrace him, for us to comfort each other and cry in each other’s arms. “I don’t think I want to have sex anymore with you. I want a divorce,” He said flatly. I sprang up in the bed, “What? Why?” Propping up on his pillow, he took a deep breath and explained, “I know you want kids. I can’t give that to you, and I love you enough to let you go find someone who can do that for you. I’ll be fine.” “But, I’ve told you, I didn’t marry you for your sperm. I married you for you. Do I want children? Absolutely. But I want our children, not someone else’s. I want to know what we look like. Me and you.” There was an urgency in my voice that caused me to tremble. A knot formed in my throat. I understood he was only trying to protect me, but he was breaking my heart at the same time. Instead, he turned his back to me and looked at the wall “No. I’m straight. I can’t live knowing I can’t give you what you want.” “You’re just angry,” I reasoned. “Maybe we should talk to someone, tell our parents.” “No!” He shouted, turning back to face me so I understood how serious he was, “I’m not telling anybody my dick don’t work! And, you can’t tell anyone either. It’s my issue, not yours.” “Well, I’m not going to leave you, especially not when you need me.” “Like I said,” he turned his back again, “this is my issue. You can have a baby with someone else. I can’t.” My tears came quickly. The knot moved from my throat to my chest, making it difficult for me to say anything in response. When I found my voice, I told him repeatedly that I loved him and that I wouldn’t leave. My pleas fell on deaf ears and he finally rolled over, pulled up the covers, and turned out the light. I sat in that dark room sobbing. I knew he didn’t mean what he was saying. I knew he was hurt, but so was I. I wanted to be a mom but that was taken away from me, and there was nothing I could do about it. I wiped my nose with my pajama shirt sleeve and looked up at the fan, focusing on the hum of the blades. It calmed me, and the coolness dried some of my tears. Without warning, I had gone from being a wife and a hopeful mom to a childless divorcee. I didn’t know if my husband and I were actually growing apart or if we just didn’t know how to handle this situation. I listened to my husband’s rhythmic breathing and wondered if he was asleep or lying awake like I was. I couldn’t imagine a life without him. The more I considered his threat to divorce me, the more panicked I became until I couldn’t lie in the bed anymore. I got up and ran to the basement where I could cry without him hearing me. For the next few weeks, we barely spoke to each other. He didn’t bring up the divorce and neither did I, but I walked on eggshells for fear that if I asked him to talk to me he would act on his words. I desperately wanted to know what he was thinking. He was my buddy, and I was his. We needed each other, even if the tension made us feel as if we didn’t. I was furious with him, but then I also felt a tenderness towards him. Even though he wouldn’t admit it, I knew he was as hurt and scared as I was. But my understanding his feelings didn’t mean that I was ready to forgive his words. I was already mourning the idea of not having a child, now I also feared losing my husband. I couldn’t wrap my thoughts around why, of all people, this was happening to us. I hadn’t understood how devoted I was to the idea of having children and raising a family, until the option was taken away. I hadn’t even fully comprehended that the option wasn’t a possibility before I was in jeopardy of losing my marriage too. Losing the children I had only dreamed of was terrible, but losing my husband was unthinkable. In a few days, I had gone from a happily married woman to a madwoman grieving children who hadn’t yet been conceived and my once enviable marriage was on the verge of ruin. I was alone. I wanted someone to blame, someone to be angry at, someone to cry with, someone to make it all go away. But each day, the reality of the issue caused a roller coaster of shoulda-woulda-couldas, why me, why him, why us, why not, I will be fine, we will be okay, this is only temporary, maybe it’s not in the plan, and to hell with all the people walking around with babies who were unfit to be parents. I deserved a baby, we deserved a baby. And yet, we couldn’t conceive a baby. CONFESSION: I had only associated grief with the loss of the living, but what I was feeling felt like a death. I grieved over an idea—the idea that we would be parents, that I would be a mother and he would be a father. After one semen analysis, that idea died. However, there was no funeral, no memorial, no tombstone, no place we could visit, and no one to share our loss. Our grief was private. We grieved our ability to conceive our own children, and the feeling was suffocating. We were both losing our light, dying on the inside, but we had to be alive and well for the world on the outside. Living a lie of happiness was a death unto itself. I came to realize that what I was grieving over was not the semen itself, but my unmet expectations. I suffered the embarrassment of not being able to have a child naturally. I feared facing a world that looked to my husband and I as a couple who had it all together and having to admit that we didn’t have it all. I was afraid of what people would say, what people would think. My ego took a huge blow, my pride was crushed. My grief had nothing to do with my child or my husband. My grief was that my perfect world was imperfect, and I was not equipped to deal with imperfection. Stephanie James is a freelance writer living in North Carolina
Life via social media is the new reality. Whether it’s a marriage proposal, a career change, or a night out with friends, all the details of our lives are being shared on a webpage designed to judge success with “likes” and “follows.” As you lounge on your couch watching Netflix, the lives of thousands of people unfold live on your feed. While the access to the idealized and seemingly perfect lives of others can be entertaining, it can also lead to some serious self-depreciation - especially for those of us dealing with infertility. How social media affects people struggling with infertility. When it comes to social media, most of us over share. If we come across a moment in life that we feel captures or enhances our identity, we simply upload a picture of it. Therefore, it’s no surprise that our news feeds are flooded with pictures of pregnant bellies and cute little babies. People post the aspects of their lives that they feel make them them, and motherhood is something deeply connected to many people’s identity - so it is impossible to escape on social media. Unfortunately, the truth is that these never-ending photos of chubby babies can be emotionally devastating for those dealing with infertility. Scrolling through these photos can cause you to feel a great deal of anxiety. These posts can act as constant reminders of the struggles you’re facing and the loneliness you feel. It is common to experience feelings of jealousy, frustration, and isolation when you see all the photos of couples and their children on your feed. Then, to make things even worse, you start to feel guilty for having those feelings - you tell yourself that you’re supposed to be elated for these new parents and you question why you’re so selfish. The truth is that we all want to feel joy and happiness for the new parents on our news feed, but when you’re struggling to conceive, it’s easier said than done, so don’t fault yourself for not feeling instant joy. You may not realize it, but you’re not alone. We know that seeing all those newborn babies can make you feel alone in your struggle with infertility. While you’re not alone, social media will prevent you from making that conclusion. Because we don’t openly discuss it, rates of miscarriage in the US are higher than many realize - with approximately 1 in 4 pregnancies ending in miscarriage each year. When it comes to struggles with infertility, approximately 6.7 percent of married women aged 15 to 44 are infertile, while 12.1 percent suffer from impaired fecundity. In addition, 12 percent, or 7.3 million women, have used fertility services to help get pregnant. In our society, these have always been taboo subjects and this has been carried over into the sphere of social media. While, yes, these are delicate matters, we constantly see posts about death, loss, and hardship on social media, so why aren’t we sharing about our conception struggles too? All in all, the lack of openness on social media is causing more and more women to keep their struggles private instead of connecting with others dealing with similar issues. How to combat the negative effects of social media. If you use social media, you are going to have to face photos of new parents and their babies. As mentioned before, it is unrealistic to think that these photos won’t affect you at all, so it is best to be prepared and mentally ready. Here are a few tips to help you combat any negative emotions:
For more information on living with infertility, check out Infertility Out Loud’s Resources. Tuck’s home page states: “Everything you need for a great night's sleep.” As someone who has struggled with getting a full night of sleep without interruption for most of my life, I was intrigued to learn more. Tuck is an online organization that offers everything from evidenced-based information on sleep to mattress reviews. Below is a well-researched and easy to follow article on the link between fertility and sleep. Head to Tuck.com for this and more. Fertility and Sleep Sleep and fertility are natural components of human life, but both are easily disrupted. For the 6.1 million American women who struggle with infertility, it’s possible that sleep and sleep dysfunction may play a role in their ability to conceive. New research is diving deeper into the complicated relationship between sleep and fertility for both men and women, offering insight into the delicate complexity of the reproductive cycle. In this article, we’ll look at the science behind the fertility-sleep connection, discover how sleep disorders each have their own impact on infertility, and share our favorite advice on how to improve your sleep health. How Sleep Affects Fertility The Importance of Sleep To understand why sleep has the power to impact fertility, it’s critical to also understand how important sleep is to our physical and mental health. Sleep consists of three distinct stages: light sleep, deep sleep, and REM sleep. All three are crucial for our well-being, and anything which impacts either the total amount of time spent asleep or the duration of stages can impact us in a wide range of ways. This is because we sleep for many reasons, not just one. Scientists are still studying the various benefits of sleep, including:
CDC initiatives suggest seven hours of sleep a night for adults over the age of 21, but a third of Americans fall short of this goal. Signs indicate that poor sleep becomes more prevalent as we age, as a study of Americans over the age of 50 found that only 32% reported getting enough sleep. Aside from their impact on fertility, sleep deprivation and sleep dysfunction are associated with a long list of ailments. These include daytime exhaustion, mood disorders (such as anxiety and depression), weight gain, a higher risk of disease (including cardiovascular disease, type 2 diabetes, and cancer), memory problems, and higher levels of stress hormones and inflammation markers. Given the importance of sleep and the impact poor sleep can have on your mind and body, it’s no surprise that sleep also plays a role in fertility. What Is Infertility? The American Society for Reproductive Medicine defines infertility as “the failure to achieve a successful pregnancy after 12 months or more of appropriate, timed unprotected intercourse or therapeutic donor insemination.” In women over the age of 35, the time limit may drop to six months. American women have an infertility rate of approximately 15.5%. This number climbs to 24.3% for women who have never previously given birth. Another study estimates that around 6.1 million American women have struggled with infertility to some degree. There is no one cause of, or treatment for, infertility. As we’ve covered, fertility is the result of a complicated coordination of bodily processes and hormones in both men and women. Just as the causes of infertility vary widely between individuals, so do treatments. However, if you struggle with sleep dysregulation or a sleep disorder, it is possible that poor sleep or circadian rhythm dysfunction is impacting your fertility. How Sleep Impacts Fertility in Women Fertility, like sleep, is a complicated process. The finely-tuned mechanisms of the reproductive cycle are still being studied, as is sleep, so the places where they interact are still in the early stages of research and understanding. However, initial studies are clear on the link between sleep and fertility. The Menstrual Cycle & Hormones Sleep can have an effect on hormones, but the menstrual cycle itself can cause fluctuations to circadian rhythms in addition to having an impact on overall sleep quality. While menstruating women without pain report sleep disturbances, these complaints worsen in severity for women suffering from premenstrual syndrome or menstrual pain. Pregnancy can also cause similar sleep health problems. In the other direction, poor sleep, sleep deprivation, and circadian rhythm disruptions can all impact hormone levels in ways which are not yet fully understood. The majority of research on the subject has focused on the impact of circadian rhythm disruptions. Shift workers, for instance, have long been known to have prolonged menstrual cycles and more incidence of abnormally heavy flow and severe menstrual pain. Melatonin, a hormone associated with the sleep-wake cycle, is thought to be a potential cause of these effects. Shift workers are known to have abnormal melatonin levels when compared to the general population. In addition to sleep, melatonin also influences the immune system, controls reproductive hormones, and may play a role in egg fertilization and embryo viability. Other Hormones Of course, melatonin is not the only hormone involved in sleep and fertility. Research on the interaction between estrogen and circadian rhythms has been limited but may also prove to be important. “Clock genes” are related to the expression of circadian rhythms as well as successful reproduction, and estrogen is known to modify the effect of these genes in the reproductive system. One sign that estrogen and circadian rhythms are further linked is that polycystic ovary syndrome (PCOS), a significant cause of infertility in women, is associated with both disordered sleep and abnormal estrogen levels. Two other hormones which are being studied in the context of sleep and fertility are prolactin and follicle-stimulating hormone (FSH). Like melatonin, prolactin is secreted from the pituitary gland. While its name references its role in prompting lactation, prolactin also affects fertility and fluctuations are associated with PCOS and lack of normal ovulation. As with many other hormones, prolactin is released at higher levels during sleep and production is suppressed by sleep dysfunction and poor sleep quality. FSH, on the other hand, has a less obvious connection to sleep. However, levels of FSH were 20% lower in women who slept for less than seven hours a day when compared to women getting enough sleep, even when factors like age and weight were accounted for. Both abnormally high and low levels of FSH are known to have profound reproductive effects. Finally, the mental impact of sleep can’t be discounted when considering the relationship between sleep and fertility. Sleep dysfunction is associated with an increased risk of mood disorders such as depression and anxiety. While the impact of mental health on the reproductive cycle is also an area in need of further study, some research has shown that anxiety and distress can lead to lower rates of pregnancy. How Sleep Impacts Fertility in Men Although male fertility is not as complicated as female fertility, it is still complex enough to affect sleep and sleep problems. Not sleeping enough and sleeping too much are both associated with male fertility problems. Men in these categories were 42% less likely to conceive with their partner, while men who reported having problems sleeping more than half the time were 28% less likely to conceive. There may be several reasons for this effect. Low levels of testosterone, for example, are known to result in a lower sperm count. Like other hormones, testosterone can be influenced by a wide range of factors. Sleep deprivation and stress are both known to result in low testosterone levels. Another potential culprit is anti-sperm antibody (ASA) production. In one study of men who fell asleep past midnight, ASA levels were higher than in those who went to bed between 10 P.M. and midnight. This study also showed low sperm counts and lower rates of sperm survival in the late-sleeping group. As in women, circadian rhythms also influence fertility in men. Studies with mice have shown that when “clock genes” were deleted or mutated, both circadian rhythms and reproductive abilities were disrupted in both male and female mice. While further research is needed to understand the impact circadian rhythm disruptions have on humans, we do know that male fertility is linked to the sleep-wake cycle. Semen collected before 7:30 A.M. has a much higher sperm count and concentration when compared to semen collected later in the day, as well as having a higher proportion of healthy, normal sperm. Seasonal changes also have an impact, with sperm count increasing throughout spring and decreasing in summer. IVF/Assisted Reproductive Technology and Sleep Assisted reproductive technology (ART) is best understood as a range of treatments for infertility. However, the success of these treatments can also be influenced by sleep and sleep dysfunction. FSH and Melatonin and IVF In-vitro fertilization (IVF) is the most common form of ART, while other types include intrauterine insemination and third-party assisted ART. Women undergoing IVF keep close track of their hormone levels, and research suggests that two of those hormones — follicle stimulating hormone (FSH) and melatonin — are particularly important to IVF while also being influenced by sleep. FSH is one of the hormones that controls the menstrual cycle. In the average woman, FSH levels peak just before ovulation. As previously discussed, women who sleep fewer than seven hours a night have FSH levels 20% lower than women who sleep for seven or more hours. While both high and low levels of FSH can impact reproduction in different ways, candidates for IVF are primarily concerned with abnormally high levels. The research is still ongoing as to whether high FSH levels correlate with poor IVF outcomes, but many ART clinics do not accept clients with FSH levels above a certain cut-off. In this case, it seems possible that too much sleep may be more of a concern than too little sleep, but research on sleep and FSH is still in the early stages. More research has been done on melatonin, although there is still much researchers do not know about its potential role in IVF. Oxygen and Seminal Quality with IVF In addition to influencing (and being influenced by) circadian rhythms and playing a role in the menstrual cycle, melatonin is also a powerful antioxidant. Oxygen damages cells and is particularly dangerous for embryos. In IVF the embryo is temporarily outside the womb and therefore exposed to more oxygen, so studies have begun to examine whether melatonin might offer protection against this damage. Male fertility is rarely given as much attention in IVF research, but poor seminal quality can still affect IVF success rates. Melatonin may play a role here as well, as it has been shown to improve the quality of semen samples through neutralizing oxygen and nitrogen. Studies on both animals and humans have indicated that adding melatonin results in improvements to sperm count, mobility, and viability. Sleep Levels and IVFAs with fertility in general, sleep dysfunction can also impact the success of ART treatments by affecting both physical and mental stress levels. One study showed that 45-75% of women undergoing IVF regularly slept for less than seven hours a night, resulting in both elevated inflammation markers and increased anxiety. The impact of reduced sleep on IVF success is still unknown, but researchers involved in the study believe their results show that treating sleep loss may be useful in improving IVF outcomes. Infertility and Sleep Disorders The International Classification of Sleep Disorders places sleep disorders into six major categories:
If you suffer from sleep dysfunction or believe you do, speak to your doctor. Not only will they be able to direct you towards the most effective treatment, but proper diagnosis will give you and your care team a better understanding of the effect it may have on your fertility. Obstructive Sleep Apnea (OSA) Obstructive sleep apnea is a common sleep-related breathing disorder. People who suffer from OSA stop breathing multiple times every night when the tissue and muscles of their throat become overly relaxed and block airflow. (Snoring, a common symptom of OSA, is the result of tissue and muscle vibration.) When the airway becomes blocked, blood oxygen levels decrease, which results in an increased heart rate and the possibility of waking up with a gasp to regain normal breathing. Men are at a higher risk of OSA, with rates of 3-7% in men and 2-5% in women. (Many people with sleep apnea do not realize they have the condition, making it difficult to obtain accurate numbers.) Because of this, the majority of research on OSA and fertility has focused on men. The regular lack of oxygen caused by OSA has been shown to reduce fertility and testicular antioxidants in male mice. Sperm were less mobile and more likely to be impacted by oxygen stress, but sperm levels did not appear to be affected. Erectile dysfunction is also a well-known symptom of OSA, appearing in 10-60% of men with the condition. As OSA-related erectile dysfunction is caused by blood vessel cells no longer sending the correct signals, treatment of the underlying cause is crucial. While not necessarily a long-term barrier to fertility, erectile dysfunction (and other forms of sexual dysfunction) are still considered to have an impact on fertility levels and the likelihood of pregnancy. OSA may be partially caused by (or influence) androgens, also known as “male” hormones. Androgens are present in women, but ordinarily at lower levels and with more subtle effects. The connection between androgens and OSA would explain why women with PCOS are at a higher risk of developing OSA. Luckily, OSA can be treated effectively. Treatment usually involves the use of a continuous positive airway pressure (CPAP) machine during sleep to keep the airways open during sleep. CPAP therapy has been shown to alleviate OSA-related erectile dysfunction. It also decreases prolactin levels in women. As people with PCOS are known to have increased prolactin levels, there is hope that treatment of OSA may aid in the treatment of infertility caused by PCOS. Circadian Rhythm Sleep-Wake Disorders As discussed earlier, circadian rhythms are the “inner clock” which regulate a wide range of effects in our body, including hormone production and our sleep-wake cycle. Circadian rhythm disorders (CRD) are just as complex. They include:
What all these disorders have in common is that they describe a kind of circadian rhythm dysregulation. One way to describe these disorders is that sufferers live with a kind of permanent or semi-permanent “jet lag” when compared to the rest of the population. In fact, jet lag is itself considered a (temporary) circadian rhythm disorder. There are few statistics on the prevalence of CRD. However, nearly a third of night workers meet the criteria for shift work sleep disorder, and delayed sleep-wake disorder is the most common circadian rhythm disorder treated by sleep specialists. No matter which CRD an individual suffers from, it may have an impact on their fertility. We know that night-working women show altered reproductive cycles, that the circadian rhythm has a major effect on hormone levels (particularly melatonin), and women who suffer from CRD are more likely to have poor reproductive outcomes. So, although we do not yet know the full effect of CRD on fertility, the connection is clear. While research has indicated a circadian rhythm component to male fertility, the majority of CRD-related fertility research has centered on women. This focus continues past conception, and some studies have found that babies born to shift-working mothers had significantly lower birth rates when compared to the children of mothers who worked during the day. Treatment for circadian rhythm sleep-wake disorders differs depending on the disorder in question. Light therapy, behavioral therapy, and doctor-prescribed melatonin supplements are all common treatments and can contribute to a far healthier sleep-wake cycle. Insomnias Insomnia can be short-term (lasting under three months) or chronic (lasting over three months), and can indicate sleep-onset insomnia (difficulty falling asleep) or sleep-maintenance insomnia (difficulty staying asleep). Whatever form it takes, insomnia is the most common sleep disorder, affecting some 60 million Americans. 40% of women and 30% of men will experience insomnia in their lifetime. Like infertility, insomnias can be caused by a wide range of biological, mental, environmental, and lifestyle factors. Everything from anxiety, to blue-light exposure, to medication, to underlying disorders can cause forms of insomnia. In terms of insomnia’s relationship with infertility, the cause is less important, unless it is due to an underlying issue with its own effect on fertility. (Infertility can also be the cause of insomnia itself, as anxiety and depression are common among infertile couples and are known to cause or worsen insomnia.) Women with insomnia have been found to struggle with infertility at rates four times those of women who sleep normally. This was true even when controlling for age, weight, and health complications, but the chronic health problems associated with insomnia can also have their own impact. One theory to explain insomnia’s impact on fertility is that it has to do with the immune system. Sleep loss is known to increase inflammation and suppress the immune system. One of the markers used to measure these effects is also seen at high levels in women with unexplained infertility, indicating a possible relationship. The treatment of insomnia is highly dependant on the individual. Cognitive behavioral therapy, medication, lifestyle changes, and other therapies can be used individually or together. Since insomnia can be caused by so many factors, it’s crucial to understand the basis of your own insomnia in order to treat it effectively. Improving Your Sleep Hygiene Sleep hygiene refers to your bedtime habits and rituals. Each person has their own sleep routine, but good sleep hygiene starts with going to bed at a set time every night and then supporting sleep with healthy routines, lifestyle changes, and a bedroom set up to encourage high-quality sleep. Along with the treatment plan suggested by your medical team, there are techniques you can use to improve your sleep health whether or not you suffer from a sleep disorder. Lifestyle Changes
Sleep Routines
Conclusion Fertility is a complicated process which can be impacted by many different elements. Although the relationship is not yet fully understood, it’s clear that sleep is one of those factors. We hope this article has helped you understand the ongoing research into this topic, as well as steps you can take to improve the quality of your sleep. It’s important to remember that effective treatments are available for sleep disorders. Speak to your doctor about any concerns you have about your sleep health. Not only will you sleep better, but your care team will have a clearer picture of your fertility journey. Jenny Silverstone created MomLovesBest.com in order to offer new mothers the advice they need when the doctors office is closed. At MomLovesBest,com, you'll find accurate, well-researched information from doctors, nurses, and other mom with real-life experiences. It's a judgement-free zone covering everything from trying to get pregnant to the parenting questions you didn't know you'd need to ask. Jenny knows first hand what it takes to become a parent and wants you to know that there is quality help available when you need it!
Below is a handy graphic you can find on MomLovesBest.com that offers some solid info on trying to get pregnant:  Chiemi Rajamahendran is a wife, a mom of 2, and founder of MissConception Coach. MissConception Coach was born out of the passion and dedication to offer love, support and guidance to women TTC and experiencing Infertility issues. She experienced and witnessed firsthand the isolation created by going through treatments and loss and vowed to make this experience a better one for others. She considers it her life passion-to offer online support to women no matter where they are in their journey, or in the world! Chiemi says: “I want every sister to know she is seen, she is heard and is not alone. I want to make sure every sister can receive support in the comfort of their own home, where they feel safe and the most comfortable. Our sisterhood of support and guidance is tailored to those experiencing stress and anxiety related to Infertility and related procedures such as IUI/IVF." Read below to learn more about Chiemi and Miss.Conception Coach, and then head to the below links to see for yourself how her noble life goal has helped so many. MissConception.Coach.com Bloom Essentials What inspired you to start Miss.Conception Coach? After witnessing and experiencing how isolating ttc and experiencing loss can be. I saw such a hole in our support system from the medical side to the 'after'. I know what I needed wasn't there and I knew the support that really helped me was from friends, and an inner circle of people who had experienced something similar. I wanted to facilitate that same sort of environment of women supporting other women in a safe, private community. Your bio on Instagram reads: “We are changing the conversation about #infertility.” As someone trying to get people to talk out loud about infertility, I really connect with this idea. How do you hope to change the conversation? By encouraging sisters to speak about how they are feeling, even if those feelings are jealousy, anger, fear, shame or sadness. I want to help them understand that it’s ok to feel these things and not to feel guilty! To acknowledge it is totally ok. It’s normal to process these feelings- they don't make you a bad person. You can own them and know that your rock bottom moments can be inspiring and powerful! They can inspire other women who might feel embarrassed about feeling them too and reassure them that is 100% normal. Sharing these hard feelings only prove the incredible amount of courage and strength inside someone fighting infertility. Miss.Conception Coach advocates connection and you facilitate private groups for people dealing with infertility. How have you found this to be helpful for people in need? What would you tell someone who is interested in reaching out but might be nervous about doing so? It's HUGE! When you ask someone on the other side of infertility what was the #1 thing that helped you survive that time, their answer is always “the support I got from other women experiencing the same thing.” It's so true! Even if via online, it is the daily, safe, familiar connection of having that group there that really carries us. I made a new group because so many members were now pregnant and wanting to continue that friendship and support! Now we have a whole separate group called Bump To Bottles. It's been amazing watching the journeys of these women who started together years ago, and now have toddlers! We do also join 'forces' with the two groups ('The Miss.Conception Coach Group' and 'Bump To Bottles.') We recently did a big surprise giveaway which the Bump To Bottles ladies hosted and donated to the Miss.Conception Group ladies! Tons of prizes and so much love and support felt showing support to the sisters still fighting. I tell anyone who I speak to, to please join our group. That there is no pressure but that I know they will get so much comfort in just being a part of that sisterhood. The Inspire section on your website offers posts about infertility and personal experiences. Has there been one post in particular that you’ve found that people seem to connect with most? Yes! The post I did last Summer: Status Updates Women With Infertility Want To Post On Social Media But Don't went viral! It is first hand shares from sisters, speaking the truth about what they go through on a daily basis. For example: 'Crappy day; after spending 10k and giving myself daily injections, Dr tells me my eggs are duds.' You hosted the Bloggers Online Fertility Conference in 2015, do you plan to do so again in the future? I have hosted two and they were such a wonderful experience. I'm not sure there is a third one in store but definitely something, that brings together our community again with a similar platform! I really want to start focusing on local face to face meets ups, groups and get togethers! Since starting Miss.Conception Coach, what has surprised you most about this community you’ve created? The resilience of the women in it! And the compassion and about of giving towards other's even when one is at their rock bottom. Such unconditional love and support towards one another! You also founded Bloom Fertility Body Care, the first (and only) body care line custom made for women trying to get pregnant. Can you tell me more about this revolutionary product line? Yes! I saw so many products for pregnancy and post pregnancy/babies etc., but NOTHING for women ttc, when really all natural products are the most important! I decided it was time for something just for ttc sisters. They truly deserve it more than anyone else! It is all natural body care that also has hormone balancing essential oils. I am working on the cream now and it will be launching soon! The feedback so far, from our soft launch, has been amazing and nothing but positive. Are there any words of advice you could give someone who might be at the beginning of their TTC journey? That you are doing the best you can. That it's enough! You aren't broken and don't need fixing. To keep sharing how you feel to those around you. To protect yourself and know the triggers that can affect how you feel. That's it's not selfish to put yourself first right now. You deserve all the love and support for this journey ahead. To just BE and allow for things to fill you with joy when you are feeling overwhelmed. Not to look for 'adding more' but just resting. Often after failed treatment and cycles we automatically go to “what can we do more. what did we not do enough of, and what can we fix.” Throw that away and just let you heart and soul rest. You did enough.  Egg donation has helped thousands of people a year achieve their dream of having a child. Often, these parents find it difficult to know how, when and even if they should share with their child the story of their conception. Julie Marie had a hard time finding the right resources to help her start this conversation with her own child, so, she created her own story. Please read below to learn more about the journey to the creation of this wonderful book that will surely inspire and help so many others. Like many newlyweds, my husband and I dreamed of having children. We looked forward to creating fun family traditions in a home full of love and laughter. Shortly after we started trying to conceive, I was diagnosed with the disease of infertility and we learned we were among the 1 in 8 couples who have trouble getting pregnant or sustaining a pregnancy. I was shocked to learn I had diminished ovarian reserve (DOR) and an undetectable anti-mullerian hormone level (AMH) at the age of 35. To make devastating news worse, we soon learned our insurance did not cover infertility and we would have to pay for our treatment out of pocket. We were unsuccessful with intrauterine insemination (IUI) and quickly moved to in vitro fertilization (IVF). Given my ovarian insufficiency, our plan was to have two consecutive egg retrievals in hopes of retrieving as many eggs as possible. Time marched forward as we lived in an isolating bubble of infertility treatments. Tens of thousands of dollars and several complications later, we completed our two egg retrievals which resulted in only 2 total embryos. The first embryo transfer was unsuccessful and the second transfer resulted in a heartbreaking miscarriage. Following the miscarriage, we reflected on the long and incredibly painful journey which had brought us to that point. We were not confident we would ever be able to achieve a viable pregnancy with my eggs. It was important to me that I carry the pregnancy if possible and we valued the option of my husband having a genetic link to our child. After considering our options, we decided to move forward with egg donation. Once the decision was made, a small glimmer of hope was restored. Our experience with egg donation was very smooth and, in the end, was the answer for us. I became pregnant and we are incredibly grateful to now be called Mommy and Daddy! Years of struggles inspired me to become an infertility volunteer and advocate, by both helping other women currently going through infertility and through infertility advocacy to lawmakers. My experience as a mother through the gift of egg donation inspired me to write the children’s book Happy Together, an egg donation story. Happy Together is a heartwarming book to help parents introduce the concept of egg donation to a young child. It is a story told through clear language and cheerful illustrations, I hope the book will comfort children with the assurance of being very much wanted and loved! For more information, please visit www.happytogetherchildrensbook.com or Amazon. In her brilliant article, Bethany Bray speaks to counselors in the field about the isolation and
heartbreak that often accompanies infertility and miscarriage. She writes about why these experiences can be so all-consuming and goes into depth regarding ways to help facilitate hope and healing. Please find the original article, published in the September 2015 edition of Counseling Today here: http://ct.counseling.org/2015/09/empty-crib-broken-heart/ This past summer, Facebook CEO Mark Zuckerberg and his wife, pediatrician Priscilla Chan, announced that they are expecting a baby. This celebrity baby news grabbed headlines for a different reason than most, however. The couple’s announcement included a candid acknowledgment that they had been trying to have a baby for several years and had suffered three miscarriages along the way. “It’s a lonely experience,” Zuckerberg wrote in a July Facebook post. “Most people don’t discuss miscarriages because you worry your problems will distance you or reflect upon you — as if you’re defective or did something to cause this. So you struggle on your at sharing our experience will give more people the same hope we felt and will help more people feel comfortable sharing their stories as well.” Zuckerberg and Chan’s post resonated with millions of people (witness the post’s 1.7 million “likes,” nearly 112,000 comments and 49,000-plus shares as of the end of August) and helped raise the curtain on some painful yet common issues that are rarely talked about openly. Although many people who face miscarriage and infertility feel alone or isolated, statistics show the circumstances are much more common than people may think. Miscarriage, defined as the loss of a pregnancy before 20 weeks, occurs in 15 percent of known pregnancies, according to the American Congress of Obstetricians and Gynecologists. The U.S. Centers for Disease Control and Prevention reports that about 12 percent of women ages 15 to 44 have “difficulty getting pregnant or carrying a pregnancy to term,” while an estimated 7.4 million women in that same age bracket have used fertility services. “Trying to make sense of it all is really, really challenging. The depth of the pain and the challenges you go through are hard to put into words,” says Kristin Douglas, a licensed professional clinical counselor and American Counseling Association member in Kentucky who has personal experience with infertility and multiple miscarriage losses. “You don’t ‘get over’ these kinds of losses. You work through them, but you don’t get over them.” Mourning what might have been A person or couple can’t help but think about the future, even if cautiously, after a fertility treatment or positive pregnancy test. Considerations from possible baby names to how the mother might be “showing” by a certain month naturally spring to mind. “When that is taken away” — either through miscarriage or an unsuccessful fertility treatment — “you’re not grieving the past, you’re grieving what was going to be. You’re grieving the future,” says Valorie Thomas, a licensed marriage and family therapist and licensed mental health counselor in Florida. “With pregnancy loss and infertility, each time it doesn’t happen, you’re grieving … for all the ways you were thinking it was going to be. Helping the client to see that can be eye-opening — acknowledging that it’s real, it’s a loss [and] it’s gut-wrenchingly painful.” Thomas knows this pain firsthand. She has been pregnant 10 times, but only one — her sixth pregnancy, a now 16-year-old son — was carried full term. Thomas and her husband also have a 7-year-old daughter whom they adopted. Unlike when other family members, friends or acquaintances die, miscarriage and infertility can leave clients without memories to grieve. Often, people don’t even realize that they have the right to grieve, says Thomas, an ACA member who has a small private practice and is an adjunct professor at Rollins College in Winter Park, Florida. It’s the type of loss “that’s hard to understand,” she says. “You [typically] think of a loss as something that was already here, and you’re grieving it [no longer being here].” With fertility treatment, she says, “You get the call from the doctors saying, ‘The pregnancy test was negative, we’ll see you next month,’ and they hang up,” leaving the individual or couple reeling with a flood of emotions, from anger and frustration to sadness and embarrassment. Clients who are struggling with infertility or grieving a miscarriage can present with a range of issues in a counselor’s office. Depression, anxiety and intense stress are very common, Douglas says, as are feelings of guilt, anger, disappointment, frustration and fear. It is also possible for these clients to wrestle with trauma symptoms associated with their loss, she says. It is not uncommon for couples or individuals to have experienced both infertility and miscarriage. Miscarriage, or “the inability to carry a pregnancy to term,” may be part of the infertility experience, Thomas says. But even when there is no overlap, couples who experience a miscarriage may share some of the same emotional responses as those who are having difficulty conceiving, she says, including a sense of helplessness, desperation and loss of control. Because miscarriage and infertility can be taboo subjects, clients may not realize that they can — and should — acknowledge a pregnancy loss. For example, Thomas says, perhaps a client feels “down” every autumn but doesn’t know why. It could be that she experienced a miscarriage years or even decades ago during the fall that she never processed. Professional counselors can provide help and support in a variety of ways to those who have experienced infertility or miscarriage. This might include helping clients work through the pain and stress of disappointment, self-doubt and even family or cultural expectations. It might also encompass encouraging these clients to practice self-care and teaching them coping mechanisms to help them get through the bad days. Above all, counselors must familiarize themselves with infertility and reproductive issues if they are going to be sensitive and effective helpers for these clients, says Ebru Buluc-Halper, a mental health counseling graduate student at Pace University who runs a support group for couples and individuals going through infertility. “If [a counselor] doesn’t know what they’re talking about, it’s a huge turnoff,” says Buluc-Halper, an ACA member who led a poster session on multicultural considerations in infertility counseling at ACA’s 2015 Conference & Expo in Orlando, Florida. She has friends “who were very frustrated by [a therapist’s] lack of knowledge and were turned off from therapy because they wanted to be understood. It doesn’t happen to everyone, but it does happen.” “People want to be heard and want someone to talk to,” says Buluc-Halper, who has personal experience with miscarriage and fertility treatment. “They are deeply in need of empathy and understanding, which they’re not getting from the people around them, sometimes even from their partners.” Counselors who don’t understand miscarriage and infertility — at the very least possessing a basic knowledge of the processes, terminology and biological factors surrounding these issues — risk reinjuring and alienating clients, agrees Douglas, an assistant professor of counselor education and coordinator of the counseling clinic at Murray State University in Kentucky. People who disclose their miscarriage or infertility struggles are often subject to the well-meaning but hurtful comments and assumptions of others, she says. Among the statements that are common: “If you just relax and de-stress, you’ll get pregnant”; “Just give it time, it will happen”; “At least you weren’t that far along to get attached”; “Maybe you should just adopt”; and “Maybe it’s not in your cards.” Comments such as these are often completely untrue and very upsetting to the receiver, says Douglas, who wrote her doctoral dissertation on miscarriage at the University of Wyoming. “The last thing a person wants is to talk to a counselor who is going to say some insensitive and hurtful things in response to what that person experienced,” Douglas says. “There is a fear of what a counselor might say. Are they going to say the insensitive things that everyone else says? Things that are so hurtful or that minimize the loss?” Handle with care One of the most important things counselors can keep in mind is that no two clients’ experiences are the same, says Courtney Armstrong, an ACA member with a private practice in Chattanooga, Tennessee. Each client will attach a different meaning to what she or he is going through. “Everyone’s experience with infertility is different. You can’t just make assumptions,” says Armstrong, a licensed professional counselor who accepts client referrals from a fertility clinic in her area. “You have to respect that it’s a process for people to come to terms with their infertility. It’s not something you can help them reason their way out of. You have to treat each person individually because every person is going to respond in a different way.” Counseling and therapy must also be individualized in cases of miscarriage. Douglas says she finds it much easier to talk about her first miscarriage, which involved triplets, than her second, which was a single baby. “People would never compare the death of a sibling or a parent to that of an uncle or other relative,” Douglas says, “but somehow, [people] just lump all the miscarriages together. Each failed fertility treatment is not the same either.” There is no one-size-fits-all way to address a client’s infertility or miscarriage in counseling, agrees Thomas. “It’s important that the counselor be aware [of] spirituality and traditions and culture. Your clients are bringing all of that to you,” she says. “You can’t just [use] a cookie-cutter approach.” Thomas terms miscarriage a “silent sorrow,” saying that the loss typically goes unacknowledged by society. Too often, she says, the message that women who have experienced miscarriage receive is: “Get over it. You’ll be fine. Don’t worry about it.” “But depending on your spiritual beliefs, depending on what that meant to you at the time, what it signified, what does family mean to you, what does creating a family [mean to you], how bad you wanted it — all those things play into your reaction,” Thomas says. Paying careful attention to the language the client uses can provide counselors clues about how the person is processing the loss, she says. For example, does the client say, “I was 10 weeks pregnant, and I lost the baby,” or does she use another word? If the client or couple isn’t ready to use the word “baby,” the counselor shouldn’t refer to the pregnancy that way either, Thomas advises. After going through pregnancy loss and several rounds of in vitro fertilization, Armstrong and her husband made the choice to be child free. Making that conscious decision was empowering, she says. “The choice piece is the really important part — deciding if this is the best and right thing for me,” she explains. Likewise, Armstrong says, in counseling it can be empowering for clients to find meaning and realize they still have the ability to make choices in an unwanted situation. Wanting to be a parent and wanting to be pregnant are two different things, and helping clients to uncouple those two concepts in their mind can be helpful, she says. “If they’re going to explore infertility treatment, adoption or other options, is this about having a child or having a child that’s biologically connected to you? The most important thing is that they feel they have the freedom to make a choice,” she says. Thomas’ experience with infertility caused her to rethink the assumptions she’d held growing up in a Catholic family with nine brothers and sisters. “In my family, it was just assumed we’d all have large families,” she says. “When that didn’t happen for me, I had to revisit [that] and ask myself if I’d be OK if that didn’t happen. Then I came to grips [with the realization] that you can create family in different ways. It was OK that I had other parts of myself to be a whole person. I realized that it may be different for me.” How to help Heartbreak can accompany miscarriage and infertility. But so can hope and healing. Here are a few ways counselors can help clients who are processing these experiences. Storytelling and narrative therapy: Two of the most important things counselors can provide to these clients are a listening ear and empathy. “It’s just so important to listen to their story, really listen to their story,” Thomas says. “Every one of them is so different. Each one has a different journey. Listen compassionately and really be present.” Douglas recommends inviting clients, but not pressuring them, to talk about their loss experiences, such as where they were and how they felt when they learned they were pregnant, what it was like to be pregnant, what happened during their miscarriage and what feelings they had when they learned their pregnancy was over. “Just like with other types of trauma, you want to be sensitive to not retraumatize clients by having them share their story over and over again,” she says. “But at the same time, if clients feel it would be healing to share their story, invite them to share it and process it as many times as they feel they need to. It can be healing to remember, to talk it through, to process these things with other people, especially if clients did not feel their loss was acknowledged or if they did not have the opportunity to share their story in full with anyone.” This hit home for Douglas as she wrote the narrative of her first miscarriage for her doctoral dissertation. It was the first time she had written out the entire story, start to finish, she says. Afterward, she read the four-page narrative aloud to her own counselor in a therapy session. “It was such a powerful moment. I just sobbed and sobbed as I read it,” Douglas says. “It was then that I realized I had shared my story with lots of different people but never the whole thing beginning to end — only parts. That was huge for me. I had a further glimpse into the power of story, the power of vulnerability, the power of giving voice to nebulous experiences and the power of validation. Sharing my story beginning to end was emotional but very healing.” The empty chair approach: This Gestalt technique can be helpful for processing “unfinished business” — something all too common for those who have had a miscarriage, according to Douglas. Counselors might ask clients to speak to an empty chair as if their child who was miscarried were sitting there. Or use the empty chair to have clients speak to whomever they need to — perhaps a co-worker who made an insensitive comment or a doctor who came across as callous, sterile or impersonal. The empty chair can also provide a means for clients to speak to their deity, even venting frustration or another emotion. “This can be a way to give the client a voice or provide a degree of closure,” Douglas says. “It not only helps clients work through complex feelings as they process lost hopes, dreams and frustrations, but also helps them have an important, needed voice.” Journaling and letter writing: Writing a letter can provide clients an outlet to tell their miscarried baby that they miss and love the child. Similarly, clients can write themselves a letter from the baby, Thomas says. “At some point when they’re ready, have the client write a letter from the baby to the parents. They can say, ‘I’m still here. I love you.’ That’s very healing, but it shouldn’t be done right away,” Thomas warns. “It takes time. [The parents] have to be ready for that.” Creating a journal can also help clients process a pregnancy loss by encouraging them to explore the loss and what it meant to them, Thomas says. Each experience will be different, whether it is the client’s first miscarriage or third, whether the client already has children at home, whether it was an unplanned pregnancy and so on. Expressive arts and other creative therapies: Douglas displayed copies of some of the pastel chalk drawings she created as part of her own way of coping with her miscarriage loss when she co-presented a session at the ACA Conference in Charlotte, North Carolina, in 2009. She advises counselors to pay attention to their clients’ creative interests and incorporate those interests into the therapeutic process, if appropriate. For example, if the client likes to garden, planting a tree in honor of a child who was miscarried might be healing for the client. If the client has a flair for design, perhaps she could design a bracelet with charms that represent the pregnancy. Douglas finds that expressive arts or other creative therapies not only help clients work through challenges associated with their loss, but also assist in making the intangible tangible. Douglas had one client who enjoyed scrapbooking. Creating scrapbook pages became her version of a journal and helped her find meaning in the miscarriage she had suffered. Scrapbooks or other creative projects can include ultrasound images, hospital bracelets, photos of baby gifts that were received or a narrative written by the client about what it felt like to find out she was pregnant. “One of the challenges of miscarriage is the intangibility,” Douglas says. “When you have such few items, those ‘artifacts’ such as an ultrasound photo become very important in validating your experience and your loss. You cling to those things.” Mind-body and wellness approaches: Thomas says mind-body approaches such as yoga, relaxation techniques, meditation, deep breathing, guided imagery and repeated prayer can be helpful to clients who have experienced miscarriage or infertility. In one case, Thomas used guided imagery with a client before her fertility treatment, instructing her to envision that her grandfather, who had passed away, would be with her to support her throughout the procedure. In addition, encouraging clients to pursue a wellness lifestyle, including eating healthy food, exercising regularly and getting enough sleep, can be helpful, both because of the health benefits provided and because it gives clients a new area of focus. Spending time on healthy cooking, for example, can divert a client’s energy and focus away from frustrated or anxious thoughts. Assure clients that they are working to be “in the best place they can be to ride this roller coaster,” Thomas says. The thought becomes: “I am doing the best I can to make my body healthy so I have a chance of conceiving.” Encouraging clients in the practice of self-nurturance, such as taking 30 minutes each day to do something they really enjoy, can also help refocus their energy away from the stress of fertility treatments. Thomas instructs clients to think of 10 things that they enjoy doing and that make them happy. Then she asks clients, “How many of these things are you doing? You’re allowed to enjoy things during this time. Look for ways to enjoy yourself.” Developing signals: Sometimes social situations can be overwhelming for individuals who are going through infertility or who have experienced a miscarriage. Buluc-Halper and Douglas both suggest that counselors have these clients develop a signal to let their partners or trusted friends know when they need to change the subject or take a break during social gatherings. But clients also need to be realistic about what they can and cannot handle, Buluc-Halper says. “Going through this experience is a good time in your life to put yourself first,” she says. “[When] you’re expected to show up at a dinner or a baby shower and you emotionally, truly, cannot handle it, it’s OK to put yourself first and say, ‘It’s not a good day for me.’ Put yourself in touch with what you’re feeling. You’re in such a fragile state. There are days when you wake up and you know that you can’t go, and others when you are strong enough.” Externalize the problem: Buluc-Halper suggests that counselors help clients remove the word infertile from their vocabulary. Infertility is not their identity, she explains. “We don’t say, ‘I’m cancer.’ We say, ‘I have cancer,’” she says. “Infertility doesn’t define them. It’s just part of their journey. Finding a way to externalize that does make it easier to go to the dinner, the family gathering, the baby shower, [knowing] this is just part of my journey. Everybody will go through something in their lives, and this [infertility] is one of the things that we just happen to be going through. … Everybody will find some sort of resolution, whatever that may be. As in every experience, there will be a resolution. It might not be the resolution you envision, but you will find some kind of closure.” The trusted friend: When clients are hesitant to tell family and friends about what they are going through, Buluc-Halper suggests that they pick one person, such as their mother or a favorite sister or cousin, to confide in. Ideally that person should be able to serve as a buffer when awkward or painful subjects or questions are raised at family or social gatherings. In Douglas’ case, she had a trusted friend who would intercept baby shower invitations for her, knowing she wasn’t ready to face such a baby-focused event. A cultural perspective: A client’s cultural background can play a huge role in how that person views and deals with miscarriage or infertility. At the same time, counselors should never assume that individual clients will experience these issues within the cultural norms of their respective backgrounds, Buluc-Halper says. Doing a cultural genogram with clients can help counselors get a better idea of the role that cultural background plays in a person’s life, she says. Thomas agrees, noting that she asks clients about their spirituality and family of origin at intake. “The very, very important part for all counselors to remember when working with infertility clients from a cultural perspective is to be very aware of their own cultural biases,” Buluc-Halper says. “Be cognizant not to distort the couple’s experience based on how you assume that culture perceives infertility in terms of its ideologies, in terms of its experiences or in terms of the resolution. … They might not be experiencing infertility the same way you might expect them to based on their cultural background.” Taking a break: For clients who are going through fertility treatments, each stage brings a series of decisions and procedures that can be exhausting, Armstrong says. Counselors can offer their clients reassurance that if they decide to take a break from treatments, it doesn’t mean they are giving up, she says. “Maybe take a month off, regroup and then go on to the next stage [of fertility treatment]. Tell them, ‘You’re not giving up. You’re just backing off for a minute to get some perspective and come back,’” Armstrong says. Internet forums: Numerous websites and online forums are available for people going through infertility and reproductive issues. Although these sites provide helpful information and a way to connect with and find support from other people facing similar issues, the sites can also cause clients to spend more time focusing on issues that cause them anxiety, stress or sadness. In Armstrong’s case, she stopped visiting online forums while she was undergoing in vitro fertilization because they were provoking her anxiety. Although such forums can offer support in many situations, Armstrong found they could also act as a platform to swap “horror stories” or misinformation. “Some people find them very helpful, while others find it makes them feel worse,” she says. “It helps them know that they’re not alone, but there can also be a risk because it can make them more worried.” If online forums don’t appear to be serving clients’ best interests, counselors can suggest that they take a break and attend in-person support groups instead. Support groups, whether online or in person, can play an integral role in breaking through the isolation that often accompanies experiences of miscarriage and infertility, Buluc-Halper adds. Grief: Douglas theorizes that women grieve miscarriage loss developmentally. “This is a life that would have been,” she explains, “and you will most likely grieve in different ways and different stages for what that child would have been like [as it aged]” — such as when the child would have started walking and talking or when the child would have started kindergarten. Missed milestones may be extra emotional as time passes. As a result, grief may resurface over and over again, but in different ways, complicating the healing process, Douglas says. Anniversaries: In cases of miscarriage, multiple dates can be painful, such as the day the couple found out they were expecting, the baby’s due date, the date they lost the pregnancy and so on. Counselors might suggest that clients engage in extra self-care on those anniversaries or commemorate the dates with rituals such as playing a meaningful song, lighting a candle or sending up a helium balloon with a letter inside to their miscarried child, Douglas says. Control: One of the most difficult aspects of dealing with infertility or miscarriage for clients is accepting that what has happened or is happening is largely out of their control. “A lot of people blame themselves and think, ‘I’m not doing enough or could be doing things differently,’” Armstrong says. In cases of infertility, some clients will do things to try to take control of the situation, such as cutting gluten out of their diets or taking their temperature daily. Counselors need to be sensitive to the fact that these clients may have devoted a lot of time and energy to finding different methods that might increase their chances of conception, Armstrong says. If the methods are giving them more confidence or security about their situation, that can be good, Armstrong says, but if the methods are only serving to make clients blame themselves further, that can be harmful. “Be mindful and aware of helping clients find what makes sense and what may not be influencing whether or not they get pregnant,” she says. In cases of miscarriage, Armstrong says she most often points to biology with clients. The human body is designed to abort a pregnancy that could be harmful, she says. “I really try and bring it back [to the fact] that we don’t understand all the reasons why [women miscarry], but it’s purely biological,” she says. Offering hope: Individuals receive very straightforward — and sometimes upsetting -- information from medical doctors about their infertility, including the slim percentage they may have of getting pregnant or the complications that could happen as a result, Thomas says. On the other side of that coin, a counselor’s focus on the positive can provide clients an antidote to discouragement, she says. “Hope is such a big factor. … Put [clients] back in charge of their life,” she advises. “Offer hope that there are some coping strategies [available and that the client is] a normal person responding to the struggles of creating a family. [Tell them], ‘You need to give yourself permission to be angry and cry. … Keep the faith. If you want a family, it will happen. It may just not be the way you envisioned.’” Couples: It takes two Spouses or significant others will naturally deal with miscarriage or infertility in different ways and process things at different rates. In fact, it is common for a counselor to see relationship partners who are in two very different states emotionally, Armstrong says. One partner may have already accepted what has happened, while the other is still in a bargaining stage, thinking, “Surely there is something we can do” to change the situation, Armstrong says. Counselors can help by educating couples that the grief that accompanies a miscarriage or infertility will come in waves and that each partner is likely to be at a different point along the grief spectrum. Once couples understand that it is natural to feel differently about what they are experiencing, they often express a sense of solace, Armstrong says. “They’re relieved [because] they don’t see themselves in conflict, just at different stages in the process. Then they can understand and be more patient with each other,” she says. “Help them understand that they’re in different stages and how to communicate and best support each other” wherever they are in the process. Differences in spirituality level or religious background can threaten to divide a couple during a miscarriage, notes Thomas. For example, one partner may consider a miscarried baby to have a soul, while the other does not. “Spirituality can be very healing or create a lot of conflict if they’re coming from different perspectives,” Thomas says. “One may feel it’s ridiculous to grieve, while the other feels it’s necessary. Work with them to be respectful of each [other’s perspective].” It can be helpful for counselors to suggest that a female client bring her partner to medical and therapy appointments when possible, Buluc-Halper says. It is important that the client learn to rely on her partner for support throughout the entire process, not just during times of extreme anxiety, she points out. “Partners don’t always understand how all-consuming this [infertility] experience is,” Buluc-Halper says. “You’re the one that is doing blood work, and your arm is purple from all the injections. It’s not to diminish the male experience of this, but they don’t always understand why the female can’t really detach herself from the issue.” As important as empathy is for counselors, it is equally important to teach that skill to couples, Thomas says. She often has couples hold hands as they tell each other what the miscarriage journey has been like for them. The counselor is there to assure both partners that whatever they are feeling is valid, real and quite possibly intense, Thomas says. “Give them a safe place to explore what this has been like for them — sometimes for the first time,” Thomas says. “What does that loss mean to them? [They are] really seeing each other describe what happened and how they’re feeling right now. Because they grieve differently, it’s important to validate their experience and [explain] that it may trigger some previous losses and intensity that might scare them.” “With infertility, they can get stuck and not want to move on if they’ve had a pregnancy loss and not really grieved it,” she says. “They need to slow down and experience what they need to experience before they go on to the next step.” Breaking the silence By inviting conversations about miscarriage and infertility, counselors can play an important role in removing the stigma and isolation that surround these issues. Douglas cites the example of breast cancer, a once-taboo subject that is now openly talked about and advocated for with well-publicized campaigns and fundraisers. “Invite the conversation and break the silence,” Douglas says. “Help give women and men permission to grieve miscarriage losses and give voice to those losses. Give them a safe, nonjudgmental place to share their stories. Invite those stories. Take time to listen to those stories over and over again, as many times as people need.” For more information
Bibliotherapy resources for clients and practitioners
Bethany Bray is a staff writer and social media coordinator for Counseling Today. Contact her at [email protected].  written by Carrie Alexander, The Tired Girl Originally posted on The Tired Girl (http://www.thetiredgirl.com/p/thank-you-hormones.html) on 6/22/17 I'm okay. Not like Britney Spears in 2007. But like Britney in 2017. We have both gone to dark places and seen some shit, but we are definitely on the upswing. She is good* and so am I. I have rarely hesitated spilling my sad guts here, but I have had pause to share that I am okay without children. And it's because people with children feel sorry for me when I am sad that I don't have any, but as soon as I am okay I can envision the judgment. People may think we didn't try hard enough, didn't want it bad enough. We could have adopted a child from the state, we could have gone to Russia, or Ethiopia. Could have fostered. What about surrogacy? If we had REALLY WANTED a child we could have one, some people think. So that means we must be selfish. We wanted them, but only kind of. And without discussing each individual option with people it can't be understood from the outside. I don't feel selfish. I will never be able to explain my actions to anyone that wants to challenge me. Everyone has to forage their own path through reproduction. I am plenty judgmental about a lot of things in life, but weirdly not in the realm of child rearing. You want to hoard babies from China? Great - thank God for you! You want to go into debt with surrogacy? Fabulous - I wanted a baby that looked like my husband too. Abortion? It seems pretty traumatic to carry a baby you really don't want. Keeping a baby you thought want to give up adoption? I'd want to keep my baby too. All judgment falls away when it comes to the reproductive choices people make. But for some reason I assume people with children don't have that - I don't have proof, it's just something visceral to me. There are many reasons I am okay, and the biggest reason is because I don't know what I am missing. I had Ralphie the dog and now Teddy the dog and they give me a place to put my momness and love. Everyone needs to talk baby talk at some point. But otherwise I don't know the joy I am missing by not having kids. I don't know what it's like to look at a small version of my husband that I grew in my body and felt kick. I don't know what it's like to be so sleep deprived and still feel a thud of love when a little person clings to me for comfort. And those of you with kids don't need to convince me - because the best thing I have going for me is that I don't know. I can't miss the Porsche I don't have. Or the taller height I don't possess. I have filled my life up with other things. Things that probably seem shallow or selfish or lazy to parents, but have meaning to me. I gave this process all I had and I don't have children to show for it. My life feels full and happy and meaningful. I'm okay. #thankyouhormones *Britney's "good" seems slightly more tenuous than mine. But she can comfort herself in millions of dollars, so she's got that going for her.  pregnantish is the first online magazine dedicated to helping people navigate all things Infertility. Founded by Andrea Syrtash, pregnantish offers a wealth of information on this often overwhelming and emotional process. You can find Andrea and pregnantish here: www.andreasyrtash.com and www.pregnantish.com Follow pregnantish: @pregnantish on facebook, @pregnantishmag on twitter, and @pregnantish on Instagram. You went from writing about relationships to focusing on Infertility, what led you to start pregnantish? Funny, I always say that I'm doing the same work as I've done for a decade, which is help people navigate relationship challenges. Infertility is so often pegged as a medical issue (which it is!) but it also affects relationships in the deepest way: the relationship you have with your partner (if you have one. If you don't, that's a whole other challenge!), the relationship to your family and friends and the relationship you have with yourself and your body. I created pregnantish (small p because...not yet pregnant!) because I've covered so many chapters of modern day relationships through my books, articles and TV appearances. I felt like a huge chapter of peoples' relationships, infertility, needed to be addressed. I always say that I'm credible, not clinical. I'm credible in that I'm a relationship journalist who has tracked trends, published books, coached people for a number of years while I've been going through trying to get and stay pregnant. I've had a medical issue since I was 14, when I was hospitalized with endometriosis, and always knew I may have challenges getting pregnant, but never imagined it would take so long. It's been over 7 years and almost 6 years ago I had open-stomach surgery to remove a freakishly large fibroid tumor. I was frustrated that content in this category was relegated to clinics, message boards and parenting sites. Bloggers do great work, and there are great advocacy sites out there, but I was searching for a high-quality lifestyle site to address this. There are over 7 million people going through this challenge. I didn't understand why it had to be a vertical on a parenting site and not an independent site/digital magazine dedicated to this audience. (I should also clarify that we address singles and LGBT who may not be 'infertile' but still need support as they go through fertility treatments.) At pregnantish we work with a team of professional journalists and a health book editor. I take the content we share very seriously and make sure we have premium content to serve this smart and thoughtful audience. Has there been a topic that most resonates with people? Yes! Anytime we publish articles or social posts about the misconceptions, it resonates with our audience. One of our most popular pieces is 'Stop Telling me To Look on the Bright Side' Our audience is sick of people telling them to just relax and think positively and it'll happen! They want people to know that they have a medical issue that requires more than the quick fixes people share with them. You advocate for talking openly about Infertility. Do you think there has been a shift toward others doing the same? I'm starting to see a shift, for sure. Celebrities are 'coming out' about their own experiences of miscarriage, IVF and/or surrogacy. Some brands are starting to recognize that this is a group that shouldn't be ignored. My hope is that the taboo is broken. One of the great essays on pregnantish is 'Let's Break the Taboo of Infertility.' that we launched the site with. The writer, Elissa Strauss, talked about how breast cancer used to be taboo and now it's hard to imagine as there are walks and merchandise and awareness. We imagine infertility will become more talked about ahead...it's so isolating to feel like nobody knows what you're going through. You present at many conferences and are interviewed often. What question are you most often asked? I'm asked why I created pregnantish when I already had and have a pretty comfortable credible brand in the relationship space. I just hosted a pilot for Fox in the Spring. I'm still out there regularly in the media sharing sex & relationship advice (which is sexier than infertility!), so people ask why I've moved on. It's important for me to communicate that I haven't moved on. I see infertility as a chapter of many modern-day relationships, so I want to address it. People also probably offer a lot of thoughts or unsolicited advice. What is the craziest thing someone has suggested to you? Definitely! That's the biggest pet-peeve with our audience, for sure. The craziest advice I got (last year!) was that I should just hold my legs high up in the air after sex and it'll work. It was comical, actually. After over 7 years, many treatments, surgery, pregnancy losses...I didn't realize it was that easy! :) What has been the most helpful advice someone has offered? The most helpful advice I got a few years back was that if I want to be a parent, I'll find a way." What advice would you offer to someone starting out on their Infertility journey? Firstly, not to feel badly that you have anxiety or stress. People will tell you to stop stressing, but this response is incredibly normal and expected. Practice self-care - that's critical. For some, that may mean skipping your 15th baby shower or it may mean getting a massage or speaking with a counselor. Find what comforts you. Finally, I always say that you don't need to know the how, the when or the where of it. You just need to know the what - that you'll be a parent. You'll get there. |
|
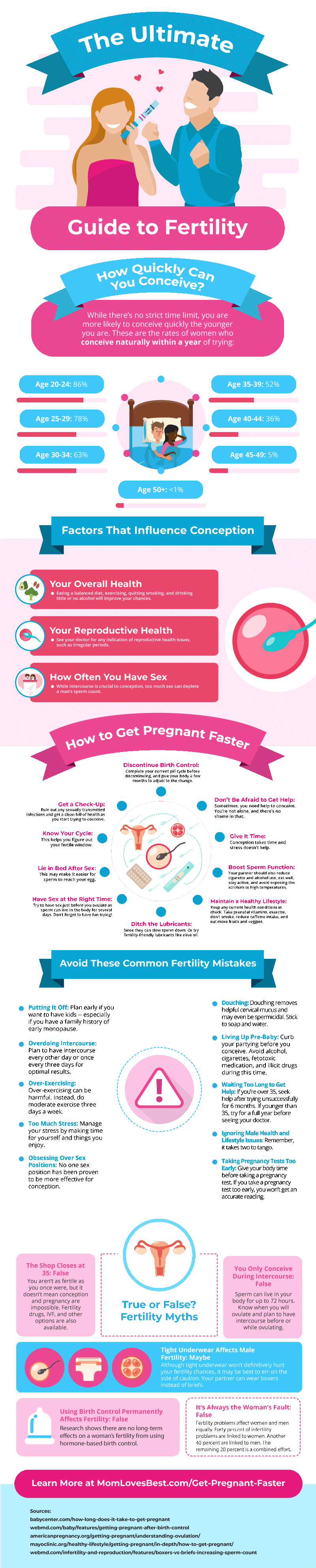
 RSS Feed
RSS Feed